2024-04-01
Beyond the ABCDEs: Exploring Additional Diagnostic Criteria for Melanoma in Skin of Colour
Share:
Melanoma is the deadliest form of skin cancer. In Canada, there were about 9,700 melanoma cases and 1,250 deaths in 2023. Melanoma is less common among people of colour, however the mortality rate is higher. People of colour are up to 4x more likely to be diagnosed with advanced melanoma and 1.5x more likely to die from the disease. The 5-year survival rate for people of colour is 70 percent, compared to Caucasians at 92 percent.
In part, this is due to the delayed detection of cancer, with people of colour receiving a melanoma diagnosis at more advanced stages. Individuals may also be unaware of their melanoma risk or how to identify potential skin cancer lesions.
Healthcare providers can decrease the impact of melanoma by familiarizing themselves with the presentation of melanoma in people with darker skin tones and promoting melanoma awareness and effective self-exams.
Melanoma may present differently in individuals with skin of colour compared to those with fair skin, including variations in colour, morphology, and distribution of lesions.
In individuals with lower Fitzpatrick skin types, melanoma lesions with characteristic asymmetries and uneven colouration are easier to identify; lesions are also typically in places exposed to sunlight, such as the arms, back, legs, and face.
For people with higher Fitzpatrick skin types, there may be less contrast between skin colour and melanoma lesions, making it more difficult to spot colour variations and irregular borders. In addition, people with darker skin tones are more likely to develop melanoma in different parts of the body. Lesions may appear on areas with lighter skin, such as the palms of hands or soles of feet, as well as on mucosal membranes.
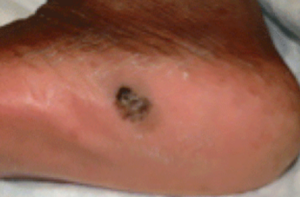
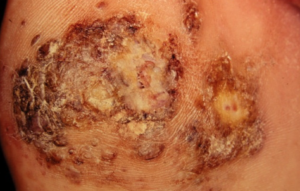
ALM is the most common type of melanoma in people with skin of colour, with a prevalence of 35-60 percent vs 2-8 percent in the Caucasian population, and is usually seen in people over the age of 40. ALM appears on the palms of the hands, soles of the feet, or beneath the fingers or toes. It begins as a flat patch of discoloured skin with variable pigmentation, resembling a bruise. Over time, it can develop into a growth or raised spot on the skin, which can become ulcerated and bleed.
ALM lesions may have distinct dermoscopic features of melanoma, including:
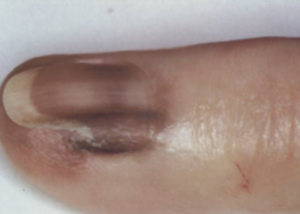
ALM occurring under the fingernails or toenails is called subungual melanoma. It typically looks like dark streaks that run vertically across the nail bed. It may be mistaken for a bruise or toenail fungus. As it progresses, it can cause the nail to break or crack.
Although ALM is the most common type of melanoma in individuals with darker skin, it is important to remember that they can still have other types of melanoma.
Mucosal melanoma appears in the mouth, throat, vagina, or anus. The location of mucosal melanoma makes it difficult to identify. They may cause symptoms similar to other conditions, leading to an initial misdiagnosis. Symptoms may include:
The standard diagnostic criteria for melanoma is the ABCDEF model. When examining a potential lesion, look for asymmetry, border, colour, diameter, evolution, and family history. In cases where the borders and colour of a lesion are indistinct, providers should pay special attention to changes over time. Noting the evolution of melanoma lesions can be one of the best melanoma screening strategies for people of colour. Follow-up visits and asking patients to take photos for comparison can help determine if a spot on the skin is changing in ways that suggest melanoma.
In cases of potential ALM, providers can use the CUBED model for skin lesion evaluation: colour, uncertain diagnosis, bleeding, enlargement, and delay in healing. A skin lesion that meets these criteria should be biopsied. When necessary, providers can work with oncologists and pathologists to request testing such as reflectance confocal microscopy and molecular diagnostics.
Clinicians have an important role in helping patients of colour by informing them about the risk of melanoma. It is essential to correct any outdated beliefs regarding skin cancer risks and provide a realistic overview of the risk of melanoma. Clinicians can also educate patients about ways to prevent melanoma and how to detect it early.
Patients should be encouraged to perform monthly self-exams and be reminded to check the areas of the body where melanomas are most likely to appear. Patients themselves detect 75 percent of melanomas. When possible, patients should see a doctor for an annual skin check. Ideally, patients should have the knowledge to self-advocate for an assessment of non-sun-exposed areas like the hands and feet.
Early detection of melanoma, followed by prompt treatment, improves survival rates and patient outcomes. This free, 30-minute accredited course, Melanoma in People With Skin of Colour: Diagnosis and Treatment, provides a comprehensive overview of current guidelines for early diagnosis in people with skin of colour.
Not an MDBriefCase member? Join today for free.
In submitting your work (the “Work”) for potential posting on the MDBriefCase Healthcare Leadership Academy website (the “Website”), you (“You”) expressly agree to the following:
Review: MDBriefCase is pleased to consider the publication of Your Work on the Website. The suitability of the Work for posting shall be determined by MDBRiefCase at its sole discretion. Nothing herein shall obligate MDBriefcase to post or otherwise publish the Work, or the maintain its posting in future.
Editing; Identification: MDBriefcase shall have the right to edit the Work to conform to our standards of style, technological requirements, language usage, grammar and punctuation, provided that the meaning of the Work is not materially altered. If posted, You will be identified as the author of the Work, or co-author if applicable.
Grant of Rights: As a condition of publication and for no monetary compensation, You hereby grant to MDBriefCase the following rights to the Work in any and all media whether now existing or hereafter developed, including print and electronic/digital formats: (1) the exclusive right of first publication worldwide; (2) the perpetual non-exclusive worldwide right to publish, reproduce, distribute, sell, adapt, perform, display, sublicense, and create derivative works, alone or in conjunction with other materials; (3) the perpetual non-exclusive worldwide right to use the Work, or any part thereof, in any other publication produced by MDBriefCase and/or on MDBriefCase’s website; and (4) the perpetual non-exclusive worldwide right to use the Work to promote and publicize MDBriefCase or its publications. The grant of rights survives termination or expiration of this Agreement.
Warranty: You warrant that the Work is original with You and that it is not subject to any third party copyright; that You have authority to grant the rights in this Agreement; that publication of the Work will not libel anyone or infringe on or invade the rights of others; that You have full power and authority to enter into this Agreement; that the Work has not been published elsewhere in whole or in part; and that You have obtained permission from the copyright owner consistent with this Agreement for any third party copyrighted material in the Work. This warranty survives termination or expiration of this Agreement.
Thank you for your interest in writing an article for the MDBriefCase Healthcare Leadership Academy website.
The Healthcare Leadership Academy welcomes submissions on all topics relevant to leaders in healthcare. Our topics include Leading in Healthcare, Leadership Lessons from COVID-19 and others. We prioritize stories that provide leadership advice to executives and managers in healthcare companies, offer actionable strategies for executing successful projects, and provide interesting angles on current healthcare topics. Submissions must be original work of the authors and unpublished. When submitting, authors represent that they have included no material that is in violation of the rights of any other person or entity.
Articles must be educational and non-promotional. If they mention the author’s company or any of the company’s products or services by name within the text, such mention should be very limited and used for reference only, not for promotion. (For example, an author might cite a survey conducted by his company but not describe his company’s product as a solution to a business problem.) Articles will be edited for clarity, style and brevity. The final headline is determined by the editor.
Guest articles for the MDBriefCase Healthcare Leadership Academy may run between 500 and 1000 words.
MDBriefCase reserves the right to accept or reject any submission and the right to condition acceptance upon revision of material to conform to its criteria.
There is no payment for contributed articles. However, MDBriefCase will give the author a byline. Authors are invited to link to the article on personal websites, corporate websites and social media platforms.
Each author understands and agrees that any submission accepted for posting is provided subject to MDBriefCase’s Author Agreement.
This website uses cookies so that we can provide you with the best user experience possible. Cookie information is stored in your browser and performs functions such as recognising you when you return to our website and helping our team to understand which sections of the website you find most interesting and useful.
Strictly Necessary Cookie should be enabled at all times so that we can save your preferences for cookie settings.
If you disable this cookie, we will not be able to save your preferences. This means that every time you visit this website you will need to enable or disable cookies again.
This website uses Google Analytics and other tools to collect anonymous information such as the number of visitors to the site, and the most popular pages. Additional information may be collected for analysis.
Keeping this cookie enabled helps us to improve our website.
Please enable Strictly Necessary Cookies first so that we can save your preferences!